Keratoconus
1. What is keratoconus?
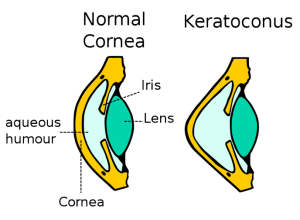
Keratoconus is an eye condition in which the cornea is shaped like a cone. The cornea is the clear tissue at the front of the eye, and acts like a camera lens to focus light on the retina. Ideally, the cornea should have a roughly spherical shape. In keratoconus, the cornea develops a cone-like shape. In fact, the word keratoconus comes from the Greek words for “cornea” and “cone.”
2. How does keratoconus affect vision?
The conical shape of an affected cornea is unable to bring images into sharp focus. Many individuals with keratoconus describe their vision as blurry, streaky, or smudged. Symptoms are generally worse at night and may include glare and halo formation around lights.
3. Why do some people get keratoconus?
The exact cause of keratoconus is uncertain and remains the topic of ongoing research. While there is likely a genetic component to the condition, many individuals with keratoconus do not have affected family members. Those with bad allergies tend to have keratoconus more frequently. It is important to note than eye rubbing may cause the condition to get worse. Therefore, those with allergies and keratoconus should consider medications to reduce itching, so they don’t need to rub their eyes.
4. How is keratoconus treated?
Mild keratoconus may be treated with glasses, just like regular myopia (“nearsightedness”) or astigmatism. In fact, many individuals with mild keratoconus are unaware that they have the condition. A careful eye examination by a doctor with expertise in this area will uncover early keratoconus. Many of my keratoconus patients have been frustrated and unhappy with their vision for years, but have never been told that they have this condition.
As the condition progresses, glasses are unable to satisfactorily correct vision, and contact lenses are the treatment of choice. Specialty soft contact lenses can be an excellent option for many individuals. These tend to be very comfortable. Gas permeable (“hard”) contact lenses are the gold standard in keratoconus treatment. The optics of a gas permeable lens can provide clear vision, even with advanced keratoconus. More recent developments in the world of contact lenses include hybrid lenses and scleral lenses.
Hybrid lenses combine a gas permeable lens with a soft lens “skirt” around the periphery. These lenses combine the benefits of gas permeable lenses (superior optics) with those of soft lenses (excellent comfort).
Scleral lenses represent an exciting solution for individuals with keratoconus. These lenses are larger than the cornea, allowing them to vault this tissue entirely. They rest on the conjunctiva, which is the white part of the eye. Scleral lenses provide unparalleled comfort and vision, even in the most advanced cases of keratoconus. These lenses require the expertise of an eye doctor with special experience in this area.
5. What if I am unable to wear contact lenses?
I hear this question commonly from patients. Fortunately, most patients (even those with advanced keratoconus) are able to successfully wear contact lenses when properly evaluated with specially designed lenses. The important part is finding an eye doctor with experience in this specific area.
6. What research is being done into keratoconus?
Several exciting technologies are being evaluated in the treatment of keratoconus. The most prominent of these is Corneal Collagen Crosslinking, or CXL. This surgical procedure strengthens the cornea to prevent further progression of keratoconus. It is currently being evaluated by the FDA in clinical trials. I generally advise patients to consider this procedure if they show evidence of progression in keratoconus. The goal would be to arrest progression, allowing long term use of contact lenses to provide good vision.
About Dr. McNulty:
Dr. McNulty has extensive experience in the diagnosis and management of keratoconus. He is a member of the Scleral Lens Education Society and a Fellow of the American Academy of Optometry.